Although fixed risk factors cannot be changed, people need to be aware of them so that they can take steps to reduce bone mineral loss as early as possible. Fixed risk factors also include disorders and medications that weaken bone and affect balance, therefore increasing the risk of fracture due to falling – read more about secondary osteoporosis.
Low bone mineral density, one of the most important indicators that a person is at risk of a fracture, is considered both fixed and modifiable since it is determined by a wide range of factors, including family history, age and lifestyle factors.
Fixed risk factors include [1]Kanis, J.A., et al., Ten year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int, 2001. 12(12): p. 989-95.
[2]Kanis, J.A., et al., A family history of fracture and fracture risk: a meta-analysis. Bone, 2004. 35(5): p. 1029-37. Kanis, J.A., et al., A family history of fracture and fracture risk: a meta-analysis. Bone, 2004. 35(5): p. 1029-37.
[3]Kanis, J.A., et al., A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res, 2004. 19(6): p. 893-9.
[4]Kanis, J.A., et al., A meta-analysis of previous fracture and subsequent fracture risk. Bone, 2004. 35(2): p. 375-82.
:
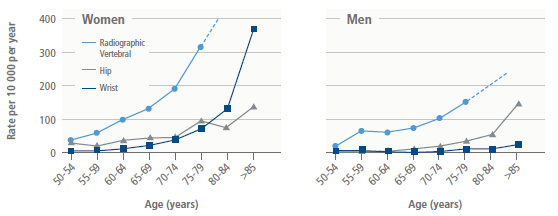
The majority of hip fractures (90%) occur in people aged 50 years or older. This is partly due to reduced bone mineral density as we age. But age can also be a risk factor independent of bone mineral density. In other words, even older adults with normal bone mineral density are more likely to suffer a fracture than younger people [1]Kanis, J.A., et al., Ten year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int, 2001. 12(12): p. 989-95.
. Read more about patients at high fracture risk.
Adapted from Sambrook and Cooper, Lancet, 2006 [5]Sambrook, P. and C. Cooper, Osteoporosis. Lancet, 2006. 367(9527): p. 2010-8.
.
Middle-aged and older men and women with annual height loss >0.5 cm are at increased risk of hip and any fracture [6]Moayyeri, A., et al., Measured height loss predicts fractures in middle-aged and older men and women: the EPIC-Norfolk prospective population study. J Bone Miner Res, 2008. 23(3): p. 425-32.
.
Women, particularly post-menopausal women, are more susceptible to bone loss than men, because their bodies produce less oestrogen. This hormone is an important component in inhibiting bone resorption/loss. Women are more likely to sustain an osteoporosis fracture than men. Lifetime risk of any fracture ranges between 40-50% in women, compared to 13-22% in men.
Osteoporosis has been shown in studies to have a large genetic component [7]Pocock, N.A., et al., Genetic determinants of bone mass in adults. A twin study. J Clin Invest, 1987. 80(3): p. 706-10.
[8]Seeman, E., et al., Reduced bone mass in daughters of women with osteoporosis. N Engl J Med, 1989. 320(9): p. 554-8.
[9]Thijssen, J.H., Gene polymorphisms involved in the regulation of bone quality. Gynecol Endocrinol, 2006. 22(3): p. 131-9.
: a parental history of osteoporosis or of fracture (particularly a family history of hip fracture) is associated with an increased risk of fracture that is independent of bone mineral density. A meta-analysis has shown the increases in risk ratios to be of 17%, 18% and 49% for any fracture, any osteoporosis fracture and hip fracture, respectively, in men and women combined [2]Kanis, J.A., et al., A family history of fracture and fracture risk: a meta-analysis. Bone, 2004. 35(5): p. 1029-37. Kanis, J.A., et al., A family history of fracture and fracture risk: a meta-analysis. Bone, 2004. 35(5): p. 1029-37.
.
After an initial low trauma fracture resulting from a simple fall, both older men and women have an increased equivalent risk of all types of subsequent fractures, especially in the next 5-10 years [10]Center, J.R., et al., Risk of subsequent fracture after low-trauma fracture in men and women. JAMA, 2007. 297(4): p. 387-94.
. A previous fragility fracture increases the risk of any fracture by 86%, compared to people without a prior fracture. Both men and women are at almost twice (1.86 times) the risk of suffering future fractures compared to fracture-free individuals [4]Kanis, J.A., et al., A meta-analysis of previous fracture and subsequent fracture risk. Bone, 2004. 35(2): p. 375-82.
[11]Klotzbuecher, C.M., et al., Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res, 2000. 15(4): p. 721-39.
. Read more about patients at high fracture risk.
Studies have found osteoporosis is more common in Caucasian and Asian populations, and the prevalence of osteoporosis and incidence of fractures of the hip and spine is lower in black than in white people.
Oestrogen deficiency caused by a defect in the hypothalamic-pituitary-ovarian axis in adolescent and young adult women afflicted by these disorders speeds up bone loss in a similar way to that which occurs in post-menopausal women, but to make matters worse, these diseases reduce the robust build-up of bone mineral density that usually occurs in adolescence and early adulthood. This may be related to both hormone imbalance and nutritional factors.
Amenorrhea has been linked to increased risk of osteoporosis [12]Fazeli, P.K. and A. Klibanski, Effects of Anorexia Nervosa on Bone Metabolism. Endocr Rev, 2018. 39(6): p. 895-910.
. Amenorrhea can be caused by intensive exercise (athletes), eating disorders (anorexia nervosa and bulimia), chemotherapy, chronic illness, Turner syndrome and/or oestrogen deficiency leading to for example premature menopause (< 45 years old). These conditions can be treated with hormone therapy in some cases.
Post-menopausal women, and those who have had their ovaries removed, must be particularly vigilant about their bone health.
Women who experience menopause before age 40 years have a higher risk of any fracture than women reporting menopause at an older age. This effect is not altered for women treated with osteoporosis therapies, suggesting that early age of menopause is an independent contributor to postmenopausal fracture risk [13]Sullivan, S.D., et al., Age of menopause and fracture risk in postmenopausal women randomized to calcium + vitamin D, hormone therapy, or the combination: results from the Women's Health Initiative Clinical Trials. Menopause, 2017. 24(4): p. 371-378.
.
Hysterectomy, if accompanied by removal of the ovaries, may also increase the risk for osteoporosis because of oestrogen loss. Investigators have also evaluated the impact of hysterectomy on long-term fracture risk. About a 20% increase in overall fracture risk is observed, but no significant effect on the typical osteoporotic fractures, defined as hip, wrist or spine fractures, collectively [14]Melton, L.J., 3rd, et al., Influence of hysterectomy on long-term fracture risk. Fertil Steril, 2007. 88(1): p. 156-62.
.