Biological causes of osteoporosis
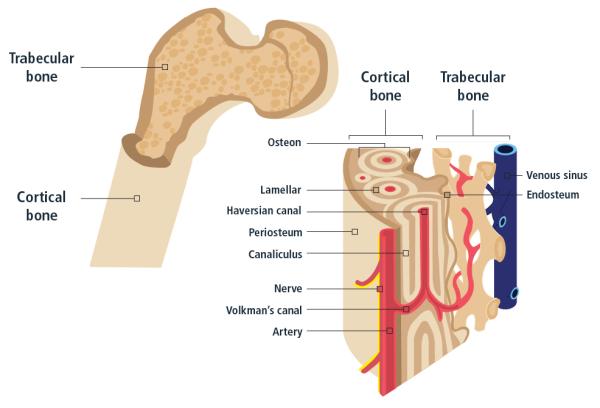
Bones are living tissue which have their own blood vessels and are made of various cells, proteins, minerals and vitamins. This structure enables them to grow, transform and repair themselves throughout life.
We are born with about 300 soft bones. During childhood and adolescence, cartilage grows and is slowly replaced by hard bone. Some of these bones then later fuse together, resulting in an adult skeleton with 206 bones.
The major functions of bones are to:
- Provide structural support for the body
- Provide protection of vital organs
- Provide an environment for marrow (where blood cells are produced)
- Act as a storage area for minerals (such as calcium)
Bones are made of two tissue types:
- Compact bone: also known as cortical bone, this hard-outer layer is strong and dense
- Cancellous bone: also known as trabecular bone, this spongy inner layer network of trabeculae is lighter and less dense than cortical bone
Bones are composed of:
- Osteoblasts and Osteocytes: these are bone forming cells
- Osteoclasts: these are bone resorbing cells
- Osteoid: this is the non-mineral, organic part of the bone matrix made of collagen and non-collagenous proteins
- Inorganic mineral salts deposited within the matrix
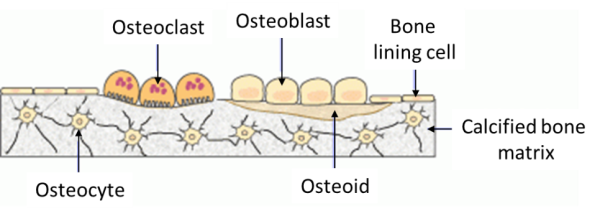
Bone Cells
Cells in our bones are responsible for bone formation, resorption, maintenance and (re-)modelling:
- Osteoblasts: These cells are derived from mesenchymal stem cells and are responsible for bone matrix synthesis and its subsequent mineralization. In the adult skeleton, the majority of bone surfaces that are not undergoing formation or resorption (i.e. not being remodelled) are lined by bone lining cells.
- Osteocytes: These cells are osteoblasts that become incorporated within the newly formed osteoid, which eventually becomes calcified bone. Osteocytes situated deep in bone matrix maintain contact with newly incorporated osteocytes in osteoid, and with osteoblasts and bone lining cells on the bone surfaces, through an extensive network of cell processes (canaliculi). They are thought to be ideally situated to respond to changes in physical forces upon bone and to transduce messages to cells on the bone surface, directing them to initiate formation or resorption responses.
- Osteoclasts: These cells are large multinucleated cells, like macrophages, derived from the hematopoietic lineage. Osteoclasts function in the resorption of mineralized tissue and are found attached to the bone surface at sites of active bone resorption. Their characteristic feature is a ruffled edge where active resorption takes place with the secretion of acid and bone-resorbing enzymes, which digest bone mineral and bone matrix.
Bone matrix
Osteoid is comprised of type I collagen (~94%) and non-collagenous proteins. The hardness and rigidity of bone is due to the presence of mineral salt in the osteoid matrix, which is a crystalline complex of calcium and phosphate (hydroxyapatite). Calcified bone contains about 25% organic matrix (2-5% of which are cells), 5% water and 70% inorganic mineral (hydroxyapatite).
Types of bone
Two types of bone can be identified according to the pattern of collagen forming the osteoid:
- Woven bone: characterized by a haphazard organization of collagen fibres and is mechanically weak
- Lamellar bone: characterized by a regular parallel alignment of collagen into sheets (lamellae) and is mechanically strong
Woven bone is produced when osteoblasts produce osteoid rapidly. This occurs initially in all foetal bones, but the resulting woven bone is replaced by remodelling and the deposition of more resilient lamellar bone. In adults, woven bone is formed when there is very rapid new bone formation, as occurs in the repair of a fracture. Following a fracture, woven bone is remodelled, and lamellar bone is deposited. Virtually all bone in the healthy mature adult is lamellar bone.
Bone development and growth
Two types of bone can be identified according to the pattern of collagen forming the osteoid:
- Woven bone: characterized by a haphazard organization of collagen fibres and is mechanically weak
- Lamellar bone: characterized by a regular parallel alignment of collagen into sheets (lamellae) and is mechanically strong
Woven bone is produced when osteoblasts produce osteoid rapidly. This occurs initially in all foetal bones, but the resulting woven bone is replaced by remodelling and the deposition of more resilient lamellar bone. In adults, woven bone is formed when there is very rapid new bone formation, as occurs in the repair of a fracture. Following a fracture, woven bone is remodelled, and lamellar bone is deposited. Virtually all bone in the healthy mature adult is lamellar bone.
Bone modelling
Modelling is when bone resorption and bone formation occur on separate surfaces (i.e. formation and resorption are not coupled). An example of this process is during long bone increases in length and diameter. Bone modelling occurs during birth to adulthood and is responsible for gain in skeletal mass and changes in skeletal form.
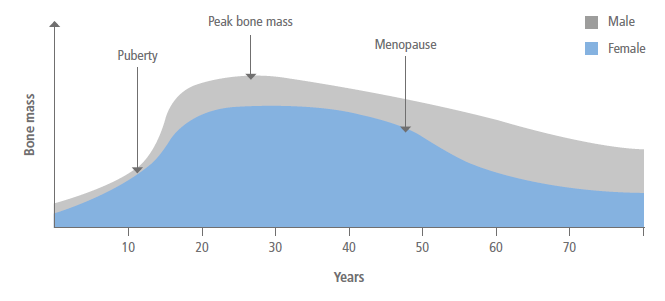
As illustrated in the figure below, peak bone mass is achieved for both males and females by the mid-twenties. Thereafter, a gradual decline into old age occurs in men, while a plateau followed by an accelerated period of bone loss for several years after the menopause occurs in women.
With the size of our skeleton and the amount of bone contained in it changing significantly throughout life, overarching objectives to maintain good bone health at various stages of life are described in prevention throughout life.
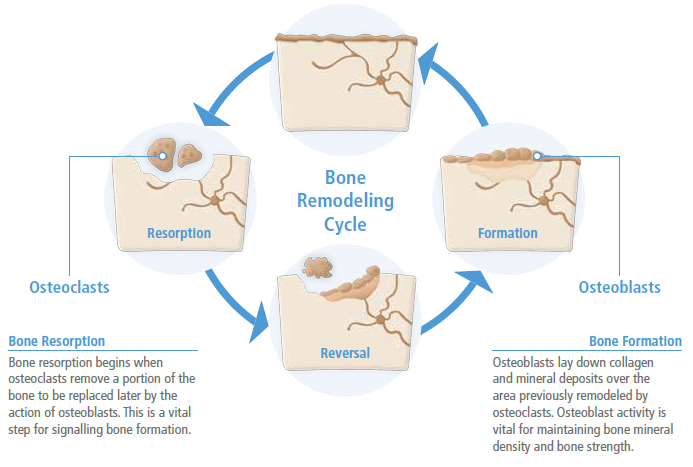
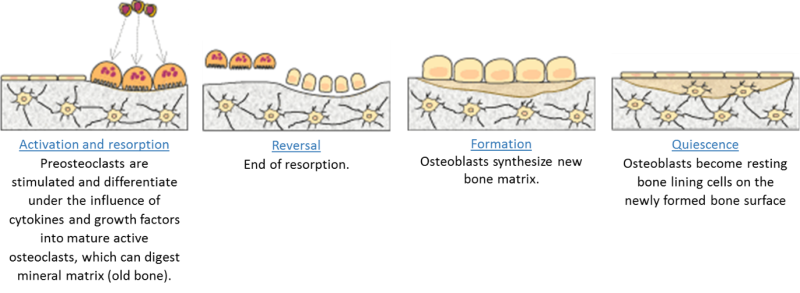
Bone remodelling
Once peak bone mass has been achieved in adulthood (described above), the bone mass and structural integrity is maintained by a process called remodelling, as illustrated in the figure below.
More specifically, remodelling is the replacement of old tissue by new bone tissue and continues throughout life so that most of the adult skeleton is replaced about every 10 years. This process involves the coupling of bone formation and bone resorption and consists of five phases as shown below.