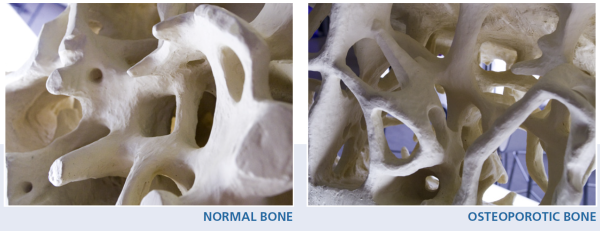
Osteoporosis is defined as a systemic skeletal disease characterized by low mineral bone mass and microarchitectural deterioration of bone tissue, more specifically a decrease in the number of trabeculae coupled to trabecular thinning and loss of connectivity, as well as decrease in cortical thickness and an increase in its porosity. This consequently increases bone fragility and susceptibility to fracture [1]Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med, 1993. 94(6): p. 646-50.
[2]Seeman, E. and P.D. Delmas, Bone quality-the material and structural basis of bone strength and fragility. N Engl J Med, 2006. 354(21): p. 2250-61.
. See bone biology.
The clinical outcome of osteoporosis is fragility fracture(s): broken bones which occur in a setting of low-level or low-energy trauma and that would otherwise not result in a fracture, such as a fall from standing height or less [3]National Institute for Health and Care Excellence NICE: Clinical Guideline [CG146] - Osteoporosis: assessing the risk of fragility fracture. 2012; Available from: https://www.nice.org.uk/guidance/cg146.
.
Given that only low bone mass can be readily measured in clinical practice, the standard operational definition for the diagnosis of osteoporosis is the finding of a T-score of ≤ −2.5 at the lumbar spine, femur neck, or total hip, by bone mineral density (BMD) testing using dual-energy X-ray absorptiometry.
However, as numerous other risk factors contribute to fracture risk in addition to BMD, it is why most guidelines now recommend that a patient with prior low-trauma fracture, or high fracture risk based on FRAX (fracture risk assessment), even without a T-score of −2.5 or lower, be considered for osteoporosis treatment. Overall, clinical judgement remains of upmost importance.
Secondary Osteoporosis
Secondary osteoporosis refers to osteoporosis caused by certain medical conditions or medications that can cause bone loss, increase fracture risk, directly or indirectly affect bone remodelling or interfere with the attainment of peak bone mass in younger individuals. Treatment of secondary osteoporosis is often more complex than treatment of primary osteoporosis, as it depends on the underlying disease.
Osteoporosis induced by medicines
Adverse effects on bone mineral density (BMD) and/or fracture have been reported for many classes of drugs. Although the link between these medicines and a decrease in BMD and/or an increase in fracture risk incidence has not always been proven as causal, evidence has been reported in the following classes of agents [4]Harvey, N.C., et al., Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int, 2017. 28(5): p. 1507-1529.
[5]Panday, K., A. Gona, and M.B. Humphrey, Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis, 2014. 6(5): p. 185-202.
:
- Androgen deprivation therapy [6]Bienz, M. and F. Saad, Androgen-deprivation therapy and bone loss in prostate cancer patients: a clinical review. Bonekey Rep, 2015. 4: p. 716.
[7]Rizzoli, R., et al., Cancer-associated bone disease. Osteoporos Int, 2013. 24(12): p. 2929-53.
- Aromatase inhibitors [7]Rizzoli, R., et al., Cancer-associated bone disease. Osteoporos Int, 2013. 24(12): p. 2929-53.
[8]Rizzoli, R., et al., Guidance for the prevention of bone loss and fractures in postmenopausal women treated with aromatase inhibitors for breast cancer: an ESCEO position paper. Osteoporos Int, 2012. 23(11): p. 2567-76.
- Glucocorticoids [9]Whittier, X. and K.G. Saag, Glucocorticoid-induced Osteoporosis. Rheum Dis Clin North Am, 2016. 42(1): p. 177-89, x.
[10]Lan, G.B., et al., Current Status of Research on Osteoporosis after Solid Organ Transplantation: Pathogenesis and Management. Biomed Res Int, 2015. 2015: p. 413169.
[11]Kanis, J.A., et al., A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res, 2004. 19(6): p. 893-9.
[12]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
- Selective serotonin reuptake inhibitors [13]Rizzoli, R., et al., Antidepressant medications and osteoporosis. Bone, 2012. 51(3): p. 606-13.
- Thiazolidinediones [14]Palermo, A., et al., Oral anti-diabetic drugs and fracture risk, cut to the bone: safe or dangerous? A narrative review. Osteoporos Int, 2015. 26(8): p. 2073-89.
- Proton pump inhibitors [15]Lau, A.N., et al., The relationship between long-term proton pump inhibitor therapy and skeletal frailty. Endocrine, 2015. 49(3): p. 606-10.
[16]Yang, Y.X., et al., Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA, 2006. 296(24): p. 2947-53.
[17]Targownik, L.E., et al., Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ, 2008. 179(4): p. 319-26.
- Certain immunosuppressants (calmodulin/calcineurin inhibitors) [10]Lan, G.B., et al., Current Status of Research on Osteoporosis after Solid Organ Transplantation: Pathogenesis and Management. Biomed Res Int, 2015. 2015: p. 413169.
- Hormone deprivation therapy [5]Panday, K., A. Gona, and M.B. Humphrey, Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis, 2014. 6(5): p. 185-202.
- Certain steroid hormones (medroxyprogesterone acetate, luteinizing hormone releasing hormone agonists) [18]Lopez, L.M., et al., Steroidal contraceptives: effect on bone fractures in women. Cochrane Database Syst Rev, 2014(6): p. CD006033.
- Certain anticonvulsants, antiepileptic drugs [19]Beerhorst, K., et al., Bone disease during chronic antiepileptic drug therapy: general versus specific risk factors. J Neurol Sci, 2013. 331(1-2): p. 19-25.
- Anti-coagulants [20]Tufano, A., et al., Oral anticoagulant drugs and the risk of osteoporosis: new anticoagulants better than old? Semin Thromb Hemost, 2015. 41(4): p. 382-8.
- Chemotherapy agents (methotrexate) [5]Panday, K., A. Gona, and M.B. Humphrey, Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis, 2014. 6(5): p. 185-202.
Other medications or chemicals that have been shown to have adverse effects include thyroid hormone treatment (L-Thyroxine), anxiolytics, sedatives, antidepressants and neuroleptics [21]Vestergaard, P., L. Rejnmark, and L. Mosekilde, Anxiolytics, sedatives, antidepressants, neuroleptics and the risk of fracture. Osteoporos Int, 2006. 17(6): p. 807-16.
, as well as certain antipsychotics (lithium), antacids containing aluminium, cigarette smoking, alcohol abuse, aluminium and barbiturates.
Associations between commonly used drug classes and bone loss and/or fragility fracture incidence are summarised below.
|
Drug class |
Loss of BMD |
Increased fracture risk |
Literature review |
|---|---|---|---|
|
Androgen deprivation therapy (ADT) |
Gonadotropin-releasing hormone agonists (GnRHs) are the most commonly used ADT. BMD declines by 2-5% during the first year of ADT. |
The risk of hip and vertebral fractures increases to 20-50% |
Bienz & Saad, 2015 [6]Bienz, M. and F. Saad, Androgen-deprivation therapy and bone loss in prostate cancer patients: a clinical review. Bonekey Rep, 2015. 4: p. 716. |
|
Aromatase inhibitors (AI) |
The annual rate of bone loss in women taking AIs is approx. 2.5% as compared to 1-2% for healthy postmenopausal women. |
Women treated with AIs have a 30% higher fracture risk than age-matched healthy women. AI users sustain more peripheral fractures than hip or vertebral fractures. |
Rizzoli et al., 2013 [7]Rizzoli, R., et al., Cancer-associated bone disease. Osteoporos Int, 2013. 24(12): p. 2929-53.
|
|
Glucocorticoids (GC) |
While all recipients of GCs are at increased risk of bone loss, older men and postmenopausal women are at highest risk with GC doses of >20 mg daily. |
30-50% of patients receiving GCs develop fractures. GC-induced osteocyte apoptosis leads to early increase in fracture risk prior to loss of BMD. |
Whittier & Saag, 2016 [9]Whittier, X. and K.G. Saag, Glucocorticoid-induced Osteoporosis. Rheum Dis Clin North Am, 2016. 42(1): p. 177-89, x. |
|
Selective serotonin reuptake inhibitors (SSRI) |
Small studies have found an association between SSRI use and bone loss. However, meta-analysis has reported SSRI-related fractures in the absence of bone loss. |
Two meta-analyses have reported the adjusted odds ratio for fracture among SSRI users to be approx. 1.7. Fracture risk is dependent on dose and duration of SSRI treatment. |
Rizzoli et al., 2012 [13]Rizzoli, R., et al., Antidepressant medications and osteoporosis. Bone, 2012. 51(3): p. 606-13. |
|
Thiazolidinediones (TZD) |
TZDs reduce bone formation through impairing differentiation of osteoblast precursors, and increase resorption through several mechanisms, resulting in bone loss. |
Two meta-analyses have reported that TZDs significantly increase fracture incidence in women with Type 2 diabetes, but not in men. Notably, fracture risk is increased in young women without risk factors. |
Palermo et al., 2015 [14]Palermo, A., et al., Oral anti-diabetic drugs and fracture risk, cut to the bone: safe or dangerous? A narrative review. Osteoporos Int, 2015. 26(8): p. 2073-89. |
Table adapted from Harvey et al., Osteoporos Int, 2017. 28(5): p. 1507-1529; with permission of Springer.
The most recurrent cause of secondary osteoporosis is glucocorticoid (GC) treatment. GCs affect the function and numbers of the three major bone cell types (osteoclasts, osteoblasts and osteocytes) [5]Panday, K., A. Gona, and M.B. Humphrey, Medication-induced osteoporosis: screening and treatment strategies. Ther Adv Musculoskelet Dis, 2014. 6(5): p. 185-202.
[22]Henneicke, H., et al., Glucocorticoids and bone: local effects and systemic implications. Trends Endocrinol Metab, 2014. 25(4): p. 197-211.
. The decrease in osteoblast differentiation and the increase apoptosis of both osteoblasts and osteocytes, in addition to the decrease in insulin-like growth factor 1 (IGF-1) due to anti-anabolic effects, all cause bone formation to be impaired [23]Canalis, E., et al., Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int, 2007. 18(10): p. 1319-28.
. As bone loss arises rapidly with GCs, fractures can occur within the first months of GC treatment, underlining the importance in managing these patients as early as possible [12]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
.
For more information on pathogenesis, prevention and treatment of secondary osteoporosis induced by androgen deprivation therapy, aromatase inhibitors and glucocorticoids, see our ‘Gaps and Solutions in Bone Health’ (pages 7-10).
Individuals who are living with a broad array of diseases can be pre-disposed to develop osteoporosis or sustain fragility fractures. A variety of conditions can increase bone loss, and fracture and/or fall risk by directly or indirectly affecting bone remodelling and/or affecting mobility and balance. Disorders that affect the skeleton include:
- Autoimmune
- Rheumatoid arthritis
- Chronic obstructive pulmonary disease (COPD) and asthma
- Chronic kidney disease (CKD)
- Digestive and gastrointestinal (read more in disorders that affect bone nutrition)
- Diseases of malabsorption (coeliac, Crohn’s, inflammatory bowel disease)
- Lactose intolerance
- Endocrine and hormonal
- Endocrine disorders (e.g. Cushing’s syndrome, hyperparathyroidism, diabetes)
- Hypogonadal states (male and female; primary or secondary; e.g. Turner syndrome/Kleinfelter syndrome, amenorrhea, Kallmann syndrome)
- Haematologic
- Neurological
- Psychophysiological disorders and mental illness
- Anorexia nervosa (read more in disorders that affect bone nutrition)
- Dementia
- Cancer
- HIV/AIDS
- Some inherited disorders
- Immobility
- Chronic disease in childhood
Evidence between common disorders and bone loss and/or fragility fracture incidence is summarised in the table below.
|
Disorder |
Evidence |
|---|---|
|
Rheumatoid Arthritis (RA) |
|
|
Chronic Obstructive Pulmonary Disease (COPD) |
|
|
Diseases of malabsorption: |
|
|
Hypogonadism |
|
|
Diabetes |
|
|
Dementia |
|
|
Chronic Kidney Disease (CKD) |
|
|
Chronic Kidney Disease (CKD) |
|