Men and women over 60-years-old are at higher risk of osteoporosis than younger people. Nevertheless, it is possible to have osteopenia (low bone mass) or osteoporosis at a much earlier age. As osteoporosis has no obvious symptoms, an evaluation of risk factors for osteoporosis (see risk factors and patients at high fracture risk) combined with a thorough medical history that includes information on any recent fractures is the first step toward a diagnosis and should indicate whether a bone mineral density (BMD) test is necessary or not. This practice is common across different healthcare systems and a few clinical guidelines even recommend a fracture risk assessment before performing a BMD test [1]National Institute for Health and Care Excellence NICE: Clinical Guideline [CG146] - Osteoporosis: assessing the risk of fragility fracture. 2012 [Accessed 22.02.2019];
https://www.nice.org.uk/guidance/cg146. The most commonly used BMD test technique is described below, however, a number of different types of test options are available – read more in other diagnostic tools.
From the pathophysiological definition of osteoporosis, it is clear that low bone mass is a crucial component of fracture risk, in addition to a number of other elements that ultimately lead to bone fragility. However, in clinical practice, bone mass is at present the unique determinant of fracture risk that can be assessed. It can, therefore, be used for diagnosis, but also to monitor treated patients. BMD is the quantity of bone per unit of volume or per unit of area.
Bone mineral density (BMD) and dual-energy X-ray absorptiometry (DXA)
As traditional X-rays cannot measure bone density and can only identify spine fractures, a bone mineral density (BMD) test must be measured by more specialised techniques. The most commonly used BMD test is a densitometric technique called DXA (dual-energy X-ray absorptiometry), which can be measured in vivo and has been validated by many studies for fracture risk assessment [2]Johnell, O., et al., Predictive value of BMD for hip and other fractures. J Bone Miner Res, 2005. 20(7): p. 1185-94.
.
DXA is a fast, quantitative technique that is capable of detecting quite small percentages of bone loss by measuring the attenuation through the body of low radiation X-ray beams with two different photon energies [3]Genant, H.K., et al., Noninvasive assessment of bone mineral and structure: state of the art. J Bone Miner Res, 1996. 11(6): p. 707-30.
, using hydroxyapatite (bone mineral) and soft tissue as reference materials. To identify the bone outline at particular sites, edge detection software is employed [4]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
.
The bone density of the whole skeleton can be evaluated, but the most commonly measured sites to assess the risk of osteoporosis using DXA are the proximal femur (and femoral neck) and lumbar spine (L1-L4). DXA technique with lateral views of the spine are used to detect vertebral fracture by vertebral fracture assessment (VFA), and recently, the trabecular bone score (TBS) has been developed also based on DXA.
DXA in the clinical diagnosis of osteoporosis
For DXA scans, the World Health Organization has defined a number of threshold values for osteoporosis. These values are based on units of standard deviation (SD) and are described as T- or Z-scores. To calculate the T-score, the recommended reference range uses femoral neck measurements in Caucasian women aged 20 to 29 years from the National Health and Nutrition Examination Survey (NHANES) III reference database [5]Looker, A.C., et al., Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int, 1998. 8(5): p. 468-89.
. For both men and women, the same female reference range is used for the diagnostic criteria.
|
Status |
Femoral neck BMD T-score (SD) |
|
Normal |
-1 and above |
|
Osteopenia |
Between -1 and -2.5 |
|
Osteoporosis |
-2.5 or lower |
|
Severe Osteoporosis |
-2.5 or lower and presence of at least one fragility fracture |
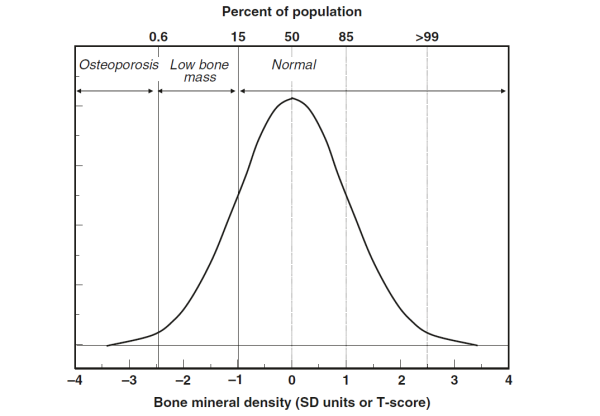
The T-score reference value being derived from bone density measurements in a population of young healthy females (see table and figure below), diagnosis of osteoporosis relies on its operational definition, which is when an individuals’ T-score for BMD at the femoral neck is equal to or more than 2.5 SDs below the reference value [6]Kanis, J.A., Diagnosis of osteoporosis and assessment of fracture risk. Lancet, 2002. 359(9321): p. 1929-36.
[7]Kanis, J.A., et al., A reference standard for the description of osteoporosis. Bone, 2008. 42(3): p. 467-75.
. In practice, osteoporosis is often defined using a T-score measured at other sites, for example at the lumbar spine [4]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
.
The Z-score reference value is derived from bone density measurements adjusted for age and sex. It therefore expresses the number of SDs that an individuals’ BMD needs to differ from the expected mean in his/her age and sex group. As such, it is mainly used to assess children and adolescents.
Threshold values for osteopenia (low bone mass) and osteoporosis are shown.
Figure taken from Ferrari & Roux, 2019 [4]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
.
Limitations
When comparing results of a same patient that has been scanned using DXA equipment from different manufacturers, caution needs to be taken as there are slight variations of important parameters between brands. These parameters include voltages used, filtering mechanisms, edge detection and soft tissue thickness adjustments. To allow comparison of results over time, patients, if possible, should be scanned using the same equipment [4]Pocket Reference to Osteoporosis, S. Ferrari, Roux, C., Editor 2019, Springer International Publishing.
.
Bone density testing by DXA is a quantitative, non-invasive, comparatively inexpensive, convenient diagnostic procedure for osteoporosis. Nonetheless, the clinical significance of osteoporosis remains the fractures that can ensue. As such, the measurement of BMD is not only a diagnostic tool, but also a risk factor assessment tool enabling clinicians to stratify fracture risk of individuals. Because of this, the advent of DXA technology has resulted in some unintended consequences(/confusion among patients and certain healthcare professionals) and there is need for a clear distinction between BMD use for diagnosis versus for risk assessment [8]Kanis, J.A., et al., European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int, 2019. 30: p 3-44
https://link.springer.com/article/10.1007%2Fs00198-018-4704-5.
Bone mineral density results showing osteopenia or osteoporosis, do not automatically mean that a fracture will ensue. In fact, most individuals who sustain fragility fractures do not have a BMD T-score below -2.5 standard deviations. The majority of fracture patients have osteopenia rather than osteoporosis as defined by BMD [9]Pasco, J.A., et al., The population burden of fractures originates in women with osteopenia, not osteoporosis. Osteoporos Int, 2006. 17(9): p. 1404-9.
. This can be explained by the fact that several non-skeletal factors impact fracture risk (read more in risk factors). In addition, as DXA only measures one of the determinants of bone strength, BMD, the other determinants described in the pathophysiological definition of osteoporosis are not considered. Despite this limitation, using DXA, vertebral or hip BMD T-scores have been shown to be a key component and tool to identify patients at increased fragility fracture risk.
When osteopenic or osteoporotic, it would be important to consider lifestyle changes and available therapies to slow down bone loss and help prevent fractures. A position paper by leading clinicians in the field also proposed that all fractures in older people should trigger secondary preventive assessment, including lifestyle, non-pharmacological and pharmacological interventions to reduce future fracture risk [8]Kanis, J.A., et al., European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int, 2019. 30: p 3-44
https://link.springer.com/article/10.1007%2Fs00198-018-4704-5. The limitations of DXA for identifying individuals who will experience a fragility fracture led to the development of the FRAX® calculator, which integrates BMD with other, at least partly BMD-independent risk factors.
Bone density testing has an additional limitation in that it provides a measure of the quantity of bone, but does not provide information on the quality of bone [10]Siris, E.S., et al., What's in a name? What constitutes the clinical diagnosis of osteoporosis? Osteoporos Int, 2012. 23(8): p. 2093-7.
. Moving forwards, new diagnostic modalities are required to englobe all the aspects of fracture risk and can readily provide clinically meaningful information relating to the determinants of bone quality, which is likely to include measures of bone microarchitecture, turnover, mineralisation and accrual of damage. To date, spinal and femoral axial DXA is still the favoured tool to diagnose and take therapeutic decisions.
REFERENCES
National Institute for Health and Care Excellence NICE: Clinical Guideline [CG146] - Osteoporosis: assessing the risk of fragility fracture. 2012 [Accessed 22.02.2019];
https://www.nice.org.uk/guidance/cg146Kanis, J.A., et al., European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int, 2019. 30: p 3-44
https://link.springer.com/article/10.1007%2Fs00198-018-4704-5