Back pain and loss of height can be the first symptoms of vertebral fractures secondary to osteoporosis. Detection and evaluation techniques for vertebral fractures include plain radiography (X-ray), vertebral fracture assessment (VFA), computed tomography (CT), magnetic resonance imaging (MRI) and nuclear bone scanning. Differences exist between these methods and are shown in the table below [1]Lewiecki, E.M. and A.J. Laster, Clinical Applications of Vertebral Fracture Assessment by Dual-Energy X-Ray Absorptiometry. The Journal of Clinical Endocrinology & Metabolism, 2006. 91(11): p. 4215-4222.
.
|
Imaging Method |
Resolution |
Radiation |
Availability |
Convenience |
Cost |
|
X- ray |
+++ |
++ |
++ |
++ |
++ |
|
VFA |
++ |
+ |
+++ |
+++ |
+ |
|
CT |
+++ |
+++ |
+ |
+ |
+++ |
|
MRI |
+++ |
0 |
+ |
+ |
+++ |
|
Nuclear scan |
+ |
++ |
+ |
+ |
+++ |
| High +++; medium ++; low +; none 0 | |||||
Spinal imaging for vertebral fracture detection.
Table adapted from Lewiecki & Laster, The Journal of Clinical Endocrinology & Metabolism, 2006 [1]Lewiecki, E.M. and A.J. Laster, Clinical Applications of Vertebral Fracture Assessment by Dual-Energy X-Ray Absorptiometry. The Journal of Clinical Endocrinology & Metabolism, 2006. 91(11): p. 4215-4222.
.
The VFA technique has been shown to be reliable and accurate in diagnosing vertebral fractures, as well as being convenient, with a decreased radiation exposure and a lower cost in comparison to the other methods available [1]Lewiecki, E.M. and A.J. Laster, Clinical Applications of Vertebral Fracture Assessment by Dual-Energy X-Ray Absorptiometry. The Journal of Clinical Endocrinology & Metabolism, 2006. 91(11): p. 4215-4222.
[2]Zeytinoglu, M., R.K. Jain, and T.J. Vokes, Vertebral fracture assessment: Enhancing the diagnosis, prevention, and treatment of osteoporosis. Bone, 2017. 104: p. 54-65.
.
Using the non-invasive imaging technique called dual-energy X-ray absorptiometry (DXA), lateral imaging of the spine can assess bone macrostructure and microstructure of the vertebrae and therefore diagnose vertebral fractures [2]Zeytinoglu, M., R.K. Jain, and T.J. Vokes, Vertebral fracture assessment: Enhancing the diagnosis, prevention, and treatment of osteoporosis. Bone, 2017. 104: p. 54-65.
[3]Genant, H.K., et al., Vertebral fractures in osteoporosis: a new method for clinical assessment. J Clin Densitom, 2000. 3(3): p. 281-90.
. Today, this method is well-established for vertebral fracture assessment (VFA) and DXA thus enables the capture of both bone mineral density (BMD) and the presence/absence of vertebral fracture(s), which are two known risk factors for fragility fracture(s) [2]Zeytinoglu, M., R.K. Jain, and T.J. Vokes, Vertebral fracture assessment: Enhancing the diagnosis, prevention, and treatment of osteoporosis. Bone, 2017. 104: p. 54-65.
[4]Klotzbuecher, C.M., et al., Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res, 2000. 15(4): p. 721-39.
.
Recommendations for VFA
Indications for VFA include older individuals, patients with historical or measured height loss, a self-reported prior fracture after the age of 50 years, kyphosis, patients on long-term glucocorticoid therapy and finally in patients at increased prevalent vertebral fracture risk [1]Lewiecki, E.M. and A.J. Laster, Clinical Applications of Vertebral Fracture Assessment by Dual-Energy X-Ray Absorptiometry. The Journal of Clinical Endocrinology & Metabolism, 2006. 91(11): p. 4215-4222.
. More detailed IOF indications for VFA or with densitometry or lateral spine imaging are show in the table below, although VFA should be considered whenever documentation of a vertebral fracture would alter a treatment decision.
|
Gender |
Indication |
|
Female |
Post-menopausal women with a T-score of -1.5 SD to -2.4 SD, and:
Post-menopausal women with a T-score of -1.5 SD to -2.4 SD, and two or more of the following: *
|
|
Male |
Men with a T-score of -1.5 SD to -2.4 SD, and: *
Men with a T-score of -1.5 SD to -2.4 SD, and two or more of the following: *
|
|
Both |
Post-menopausal women and men with osteoporosis by bone density criteria** if documentation of a prevalent vertebral fracture will influence:
Women and men of any age on chronic glucocorticoid therapy if documentation of a prevalent and/or incident vertebral fracture will influence:
|
|
*If the documentation of a vertebral fracture would influence choice of therapy. |
|
Table made with information from our Vertebral Fracture Initiative [5]International Osteoporosis Foundation: Vertebral Fracture Initiative - Part III - Densitometric Vertevral Fracture Assessment (VFA). 2011;
See link.
For more information see our manuscripts, slides and annotations in the Educational Hub.
Contraindications for VFA include [5]International Osteoporosis Foundation: Vertebral Fracture Initiative - Part III - Densitometric Vertevral Fracture Assessment (VFA). 2011;
See link:
- “Recent” imaging of the spine that can be reviewed for incident fractures (e.g. chest X-ray, CT or MRI of spine or nuclear medicine bone scans)
- Pregnancy
- When results would not alter therapy
There are multiple methods for vertebral fracture diagnosis [1]Lewiecki, E.M. and A.J. Laster, Clinical Applications of Vertebral Fracture Assessment by Dual-Energy X-Ray Absorptiometry. The Journal of Clinical Endocrinology & Metabolism, 2006. 91(11): p. 4215-4222.
:
- Quantitative, known as morphometric (by measurement)
- Usually employed in population studies and some clinical trials
- For clinical practice it is time consuming and may be too complex
- Exclusive use may result in false positives and negatives [6]Ferrar, L., et al., Identification of vertebral fractures: an update. Osteoporos Int, 2005. 16(7): p. 717-28.
- Semiquantitative (SQ), a combination of morphometric and visual assessment
- Preferred method for diagnosing vertebral fractures
- Described below, the Genant SQ method has been successful in clinical trials and clinical practice for many years [7]Genant, H.K., et al., Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res, 1993. 8(9): p. 1137-48.
- For clinical practice they can be easily applied and have been validated in comparison with other methods [8]Black, D.M., et al., Comparison of methods for defining prevalent vertebral deformities: the Study of Osteoporotic Fractures. J Bone Miner Res, 1995. 10(6): p. 890-902.
- Qualitative, by visual assessment only
- Effective recognition of vertebral fractures is possible by an experience observer
- Exclusive use is however very subjective as it is associated with high interobserver variability [6]Ferrar, L., et al., Identification of vertebral fractures: an update. Osteoporos Int, 2005. 16(7): p. 717-28.
To enable comparison between VFA reports, the method used should be stated.
In order to assess the severity of vertebral fractures, a semiquantitative method based on visual inspection was developed. It has been extensively used in clinical trials and epidemiological studies. The severity of the fracture is assessed by measuring the extent of vertebral height reduction, by its morphological changes, and by differentiating the fracture from nonfracture deformities [7]Genant, H.K., et al., Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res, 1993. 8(9): p. 1137-48.
.
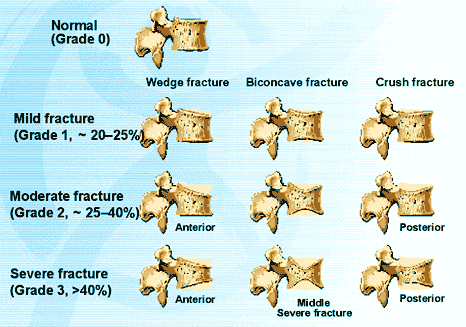
Vertebral deformities resulting from osteoporotic fractures are classified as:
- Wedge fractures: causing anterior height loss
- Biconcave fractures: causing central compression of the end-plate regions and maintenance of anterior and posterior heights
- Crush fractures: causing compression of the entire vertebral body
Grades are assigned to each vertebra based on the degree of height reduction as shown in the figure below:
- Mild or grade 1: 20–25% loss of vertebral height
- Moderate or grade 2: 25–40% loss of vertebral height
- Severe or grade 3: greater than 40% loss of vertebral height
Adapted from Genant et al., J Bone Miner Res, 1993 [7]Genant, H.K., et al., Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res, 1993. 8(9): p. 1137-48.
.
Although this method does not link the type of deformity with the grading of the fracture, one advantage of this method is by assessing the severity of the deformation, new deformities occurring on a prevalent vertebral fracture can be assessed within the range of grading.
REFERENCES
International Osteoporosis Foundation: Vertebral Fracture Initiative - Part III - Densitometric Vertevral Fracture Assessment (VFA). 2011;
See link